Problem: access
At Memorial Sloan Kettering, an oncologist team has a primary responsibility of patient care. In this model, a patient sees the primary oncologist throughout his care (unlike some other hospitals where patient can see any oncologist who are available at the moment). While patients can develop deep relationship with the primary oncology team (This is important to patients, and clinical outcomes), patient’s access to care is limited. Patients get to report their symptoms during appointment time, which is usually days or weeks after it happened. Sometimes for acute symptoms, patients wait to call their doctors until symptom develops to a critical problem, since they do not want to bother their doctors.
Idea: change in care model
To provide access to clinicians while patients are at home, there needs to be a team of clinicians who can monitor patients status and apply interventions 24/7. Using digital tools, we can minimize the interruption to patients life minimal. Asking are you doing ok? If the answer is yes, life goes on. If a patient says slight fever, a clinician can react right away, in a much more proactive fashion (than patient showing up at urgent care center with much higher fever)

^ Service model changes
Challenge: scale while not losing the benefit of relationship
The benefits are so obvious. Patients can stay home (staying more time at home leads to higher patient satisfaction), symptoms can be addressed early, less treatment courses being canceled because of severe symptoms. However, implementing a new model of care scared many of us because of the fear of losing benefits of close relationship between patients and primary oncologist.
Change management: Transformation principles
Design team who seeded this idea to the institution wanted to make sure that we are bringing positive changes into the organization, and created transformation principles with our leadership. It helped the project team stay on track throughout the development.

^ Transformation principles helped people think differently, and the institution manage changes when the impact of change was at scale.
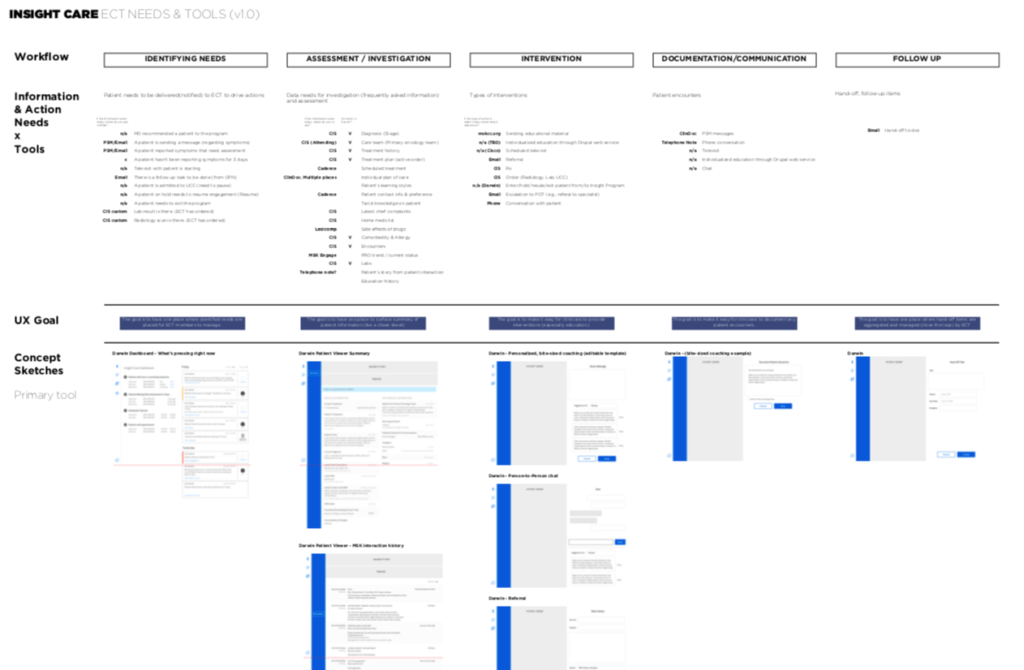
Solution: Digital service framework
I created a service interaction architecture that explains the value exchange between key actors in this care model. Connected with digital tools, patient and the monitoring team can communicate daily care needs, monitoring team and the primary oncologist can coordinate. Patient and primary oncologist can leverage the data that have been collected in between appointments when they meet in person.

^ Defined what tools do we need, the role of each tool, and feature sets to enable the service and add value to each players in the service.
Implementation: Orchestrating efforts with stories
The future that we have been dreaming through this project requires multi-level changes: building a new care team (recruiting, new job description), connecting/modifying a dozen technology systems, changing culture, and communicating it to patients and the organization. It was a big challenge to coordinate the efforts, and I proposed to tackle this challenge with a lens of desired experience, rather than operational challenges to make sure we stay focused on the key value we are creating.
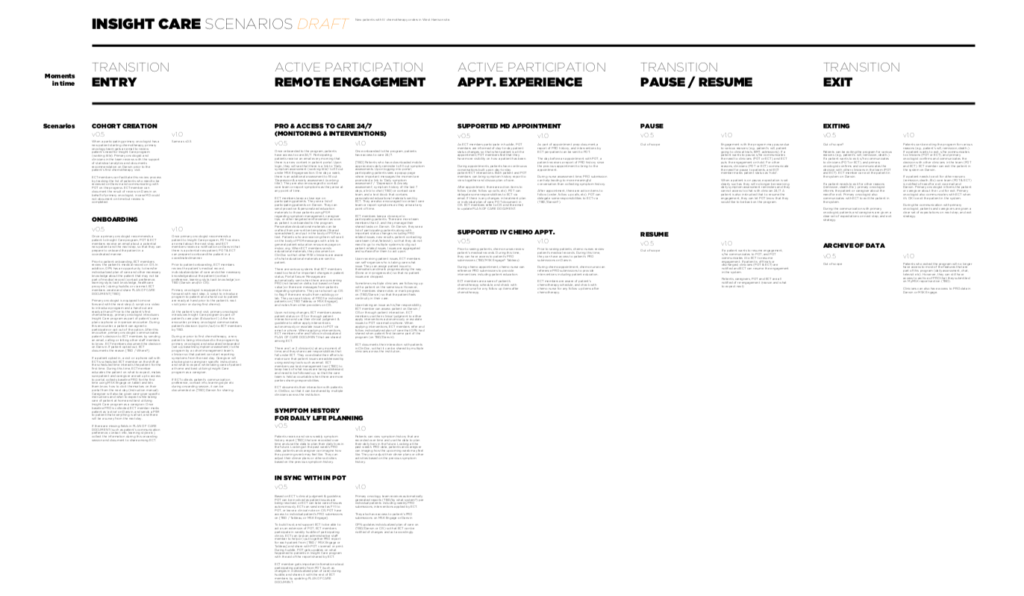
^ Considering feasibilities at each phase, I have proposed what experience can be created. We knew the first day we’d launch the pilot, we won’t be able to use seamless text based interaction, but we will be using a survey system that the institution already has. The experience from day 1 won’t be what we have dreamed of, but this way we keep our minds to the future.
Bringing empathy to the table at a systemic level
Throughout the development phase, we wanted to make sure that we are capturing diverse perspective of key actors in the service: Patient, monitoring care team, primary oncologist team, and the institution. Each has needs, pain points, and relationships with other parties. We did empathy mapping for each one to understand the interplay of them.
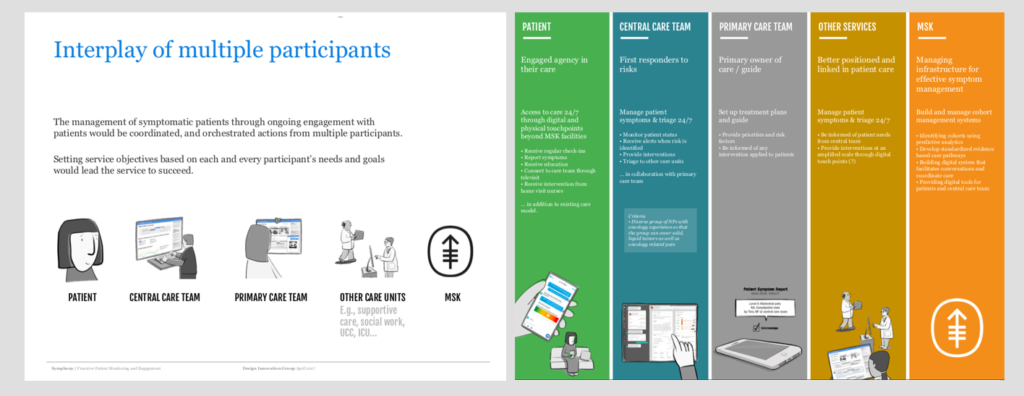
^ Cancer care is an orchestrated efforts with interconnected parties. We have looked at key players in the future scenarios and each player’s actions and values in this program.
Stay focused on patients
Upon building a foundational understanding of the interplay, we also wanted to make sure that we are designing a service that is built with patients at the center. We have asked physicians to pick patient cases who might have benefited from this type of program the most. We invited clinicians, operations staffs to discuss missed opportunities to inform the service creation.
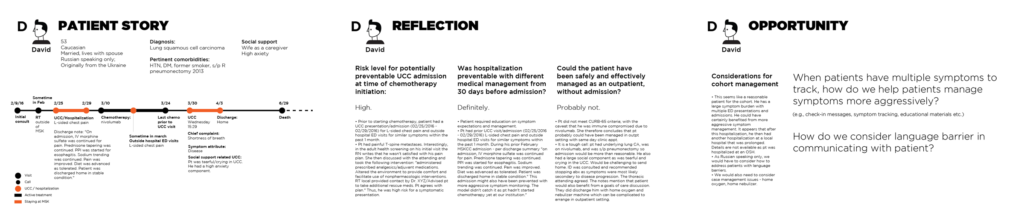
We also met with a few patients who are in active chemotherapy. We listened to their experience at home, times when they missed having access to clinical staff members, how they are tracking their symptoms and what they do with the information.
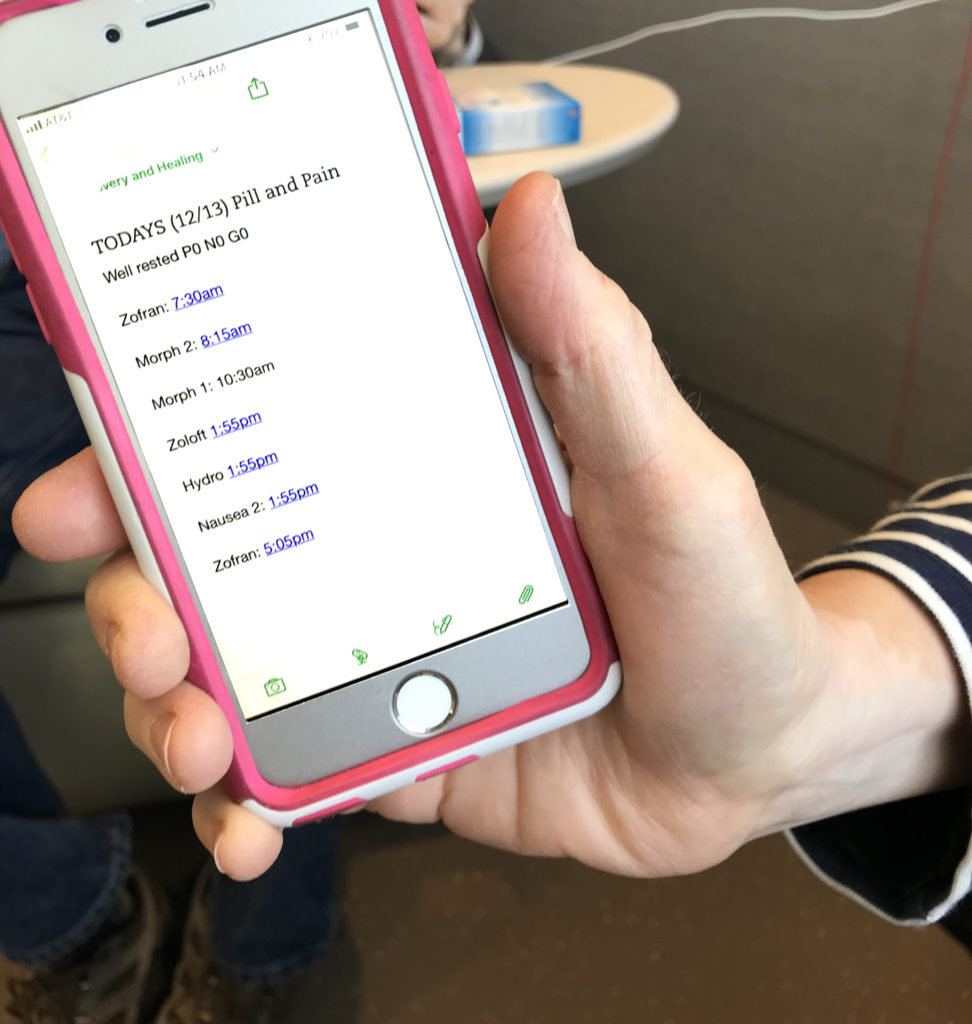
^ Interviews with patients and caregivers who are in active chemotherapy.
Brining ideas to life
Many sketches, prototypes, mockups have been made throughout the project to facilitate discussions among the project team. We mainly sketched patient side experience, and the central team’s experience as those were two major opportunities to make changes.

- Workshop – research (stakeholder interview, dealer interview, customer interview) – current state customer journey – concept framework
ROLE
- as a design lead in the project, managed multiple designers, scope, project plan …
CHALLENGE
- spread design role in large healthcare organization
RESULT
- First pilot program have been launched in October 2018 with 3 participating clinics